In the search for treatments for COVID-19, many researchers are focusing their attention on a specific protein that allows the virus to infect human cells. This protein, which cells carry on their surface, is called angiotensin converting enzyme 2 (ACE2) and provides the entry point for the coronavirus to enter cells. ACE2 is present in all people, but the quantity of this protein can vary among individuals and in different tissues and cells throughout the body.
A team of researchers including Dr. Dietrich Lorke, Professor and Chair of the KU Department of Anatomy and Cellular Biology, recently published a review into the potential impact of commonly prescribed drugs and pharmacologically active compounds on COVID-19 pathology and risk through the regulation of ACE2 levels in the body. Dr. Lorke, with Dr. Murat Oz, Kuwait University, and Dr. Nadine Kabbani, George Mason University, published their findings in the journal Pharmacology and Therapeutics.
“The emergence of COVID-19 as a global pandemic has raised concern throughout the world and spurred an urgent need for prevention and treatment,” said Dr. Lorke. “In order to enter the host cell, the coronavirus binds to an enzyme called angiotensin converting enzyme 2 (ACE2), which is found in a variety of different organs in the body, including the lungs, small intestine and the nasal cavity.”
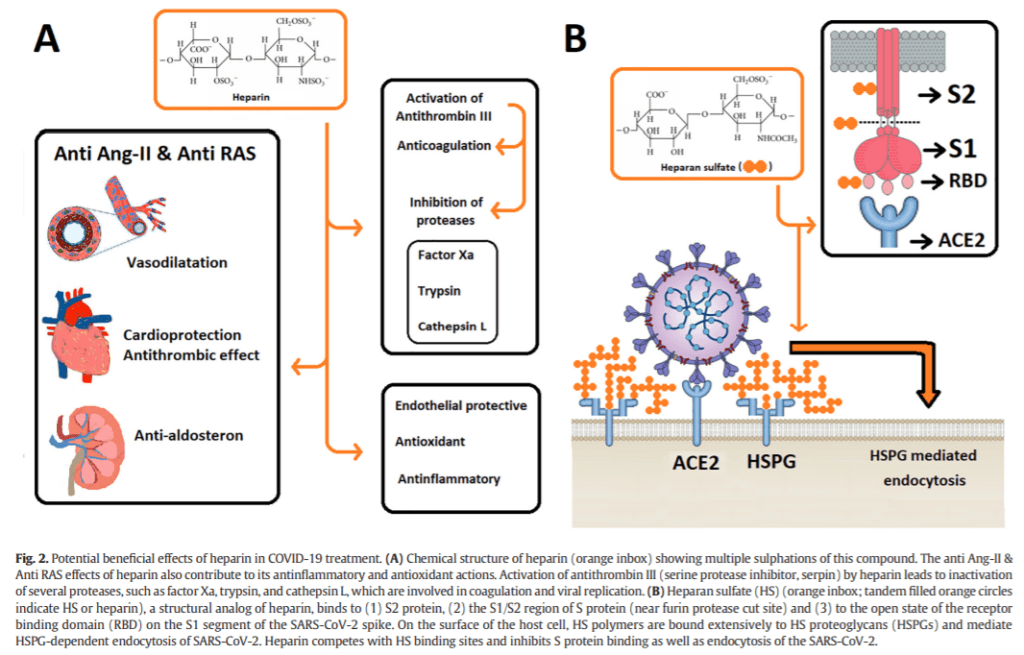
ACE2 generates small proteins that regulate functions in the cell. Using a spike-like protein on its surface, the COVID-19 virus binds to ACE2, and makes its way into the cell through this doorway. Not only does ACE2 act as an entry point for the SARS-CoV-2 virus, but its normal function also influences inflammation and cell death in the lung cells. When the COVID-19 virus binds to ACE2, this regulation is disrupted, which contributes to the lung and heart damage seen in COVID-19 patients.
It is understandable, then, that higher ACE2 expression in the body is correlated with higher infectivity, suggesting that increased ACE2 levels may predispose individuals to COVID-19. Patients with hypertension, diabetes and coronary heart disease may have higher levels of ACE2, but while the SARS-CoV-2 virus requires ACE2 to infect cells, the precise relationship between ACE2 levels, viral infectivity and the severity of a resulting infection is still a matter of debate.
Certain medications, including ACE inhibitors and Angiotensin 1-Receptor (AT1-R) blockers, have been reported to increase ACE2 expression, raising concerns regarding the safety of these drugs in patients exposed to COVID-19. This is especially concerning since both an ACE inhibitor and an AT1-R blocker are among the ten most commonly used drugs worldwide, with a combined 155 million prescriptions per year in the U.S. alone. Patients receiving these drugs would represent a substantial group of people at risk if this hypothesis proved true. However, several studies have shown that using these medications does not increase a patient’s risk of contracting COVID-19.
“The problem is that many of these observations have been made in animals and that these results do not necessarily reflect the situation in humans,” explained Dr. Lorke. “In one analysis of 12,594 patients who tested positive for COVID-19, there was no association between any single medication class and an increased likelihood of a positive test. Moreover, none of these medications were associated with an increased risk of severe illness among patients who tested positive. Several other clinical findings show similar results.”
Additionally, results from these studies suggest the use of ACE inhibitors may even have some beneficial effects on the clinical outcome of COVID-19. In small cohorts of COVID-19 patients with hypertension, the use of ACE inhibiting drugs significantly improved outcomes, with some critically ill elderly COVID-19 patients seeing lower mortality rates.
ACE2 also has some protective effects against tissue injury, the likes of which are seen in the lungs following infection with COVID-19. With the virus occupying the ACE2 receptor, the ACE2 levels in the body are reduced, which may make individuals more susceptible to severe illness from COVID-19. The ACE2 facilitates the virus getting into the body, but the decrease in available ACE2 contributes to tissue injury such as inflammation in the heart and lungs.
“ACE2 plays an important role in counteracting some of the harmful effects of inflammation in the lungs,” explained Dr. Lorke. “Unsurprisingly, a vast number of drugs significantly affect the activity and expression of ACE2. Considering the crucial role of ACE2 in coronavirus infections, the consequences of these drugs have been the subject of much recent debate. So far, evidence from the majority of clinical and epidemiological studies indicates that these drugs do not negatively affect the susceptibility and prognosis of COVID-19. It remains to be seen whether other drugs and pharmacologically active substances affect coronavirus susceptibility or disease prognosis.”
Understanding the action mechanisms of ACE inhibitor drugs is crucial for providing guidance for further clinical studies. Knowledge of the pharmacological regulation of ACE2 by various drugs and compounds also helps to better understand how these molecules work at cellular and organ system levels, particularly concerning infection with COVID-19.
The researchers report that interrupting the SARS-CoV-2 spike protein binding to ACE2 is a feasible strategy against COVID-19. They note that new drugs could be developed that bind to the active site of ACE2 and disrupt the interaction with the SARS-CoV-2 virus to prevent infection.

Leave a Reply